It’s been seven days with no Letrozole (sung to the tune of Nothing Compares 2 U).
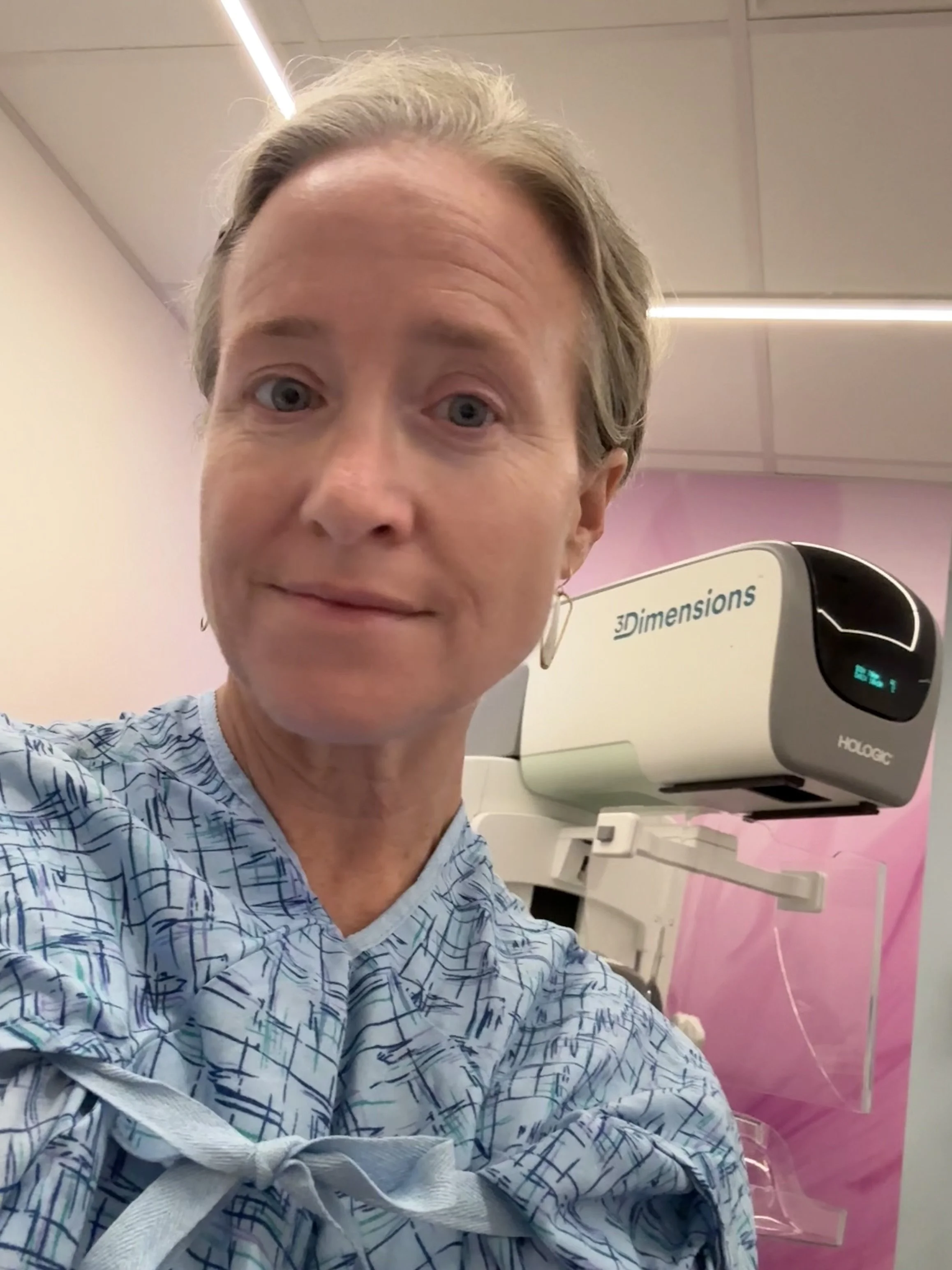
That’s the aromatase inhibitor (AI) I was taking to reduce the risk of breast cancer recurrence (by suppressing estrogen production, since my cancer was hormone positive).
I’m on a 3-4 week “vacation” from Letrozole before trying a new AI. The hope is the next one won’t cause such significant joint pain for me.
What I’m most hopeful about is how I might feel next week at this time. Letrozole has a 2-day half life, which means by approximately the two week mark, I could feel relief from symptoms. Just a smidge of estrogen. That’s all I want. I never thought I’d utter those words after my diagnosis of triple positive breast cancer.
My most significant symptom from Letrozole is joint pain. My knees are stiff and achy 24-7 and I’ve developed sciatica from my lower back down my leg and into my foot. I’m never not noticing it.
Last year, I thought, “joint pain? I can handle that. I’ve had three knee surgeries. I’ve experienced joint pain. I’ve made it through chemo. I’m tough.”
Nope. Nope. Nope. Or yes, I’m tough. But Letrozole is tougher.
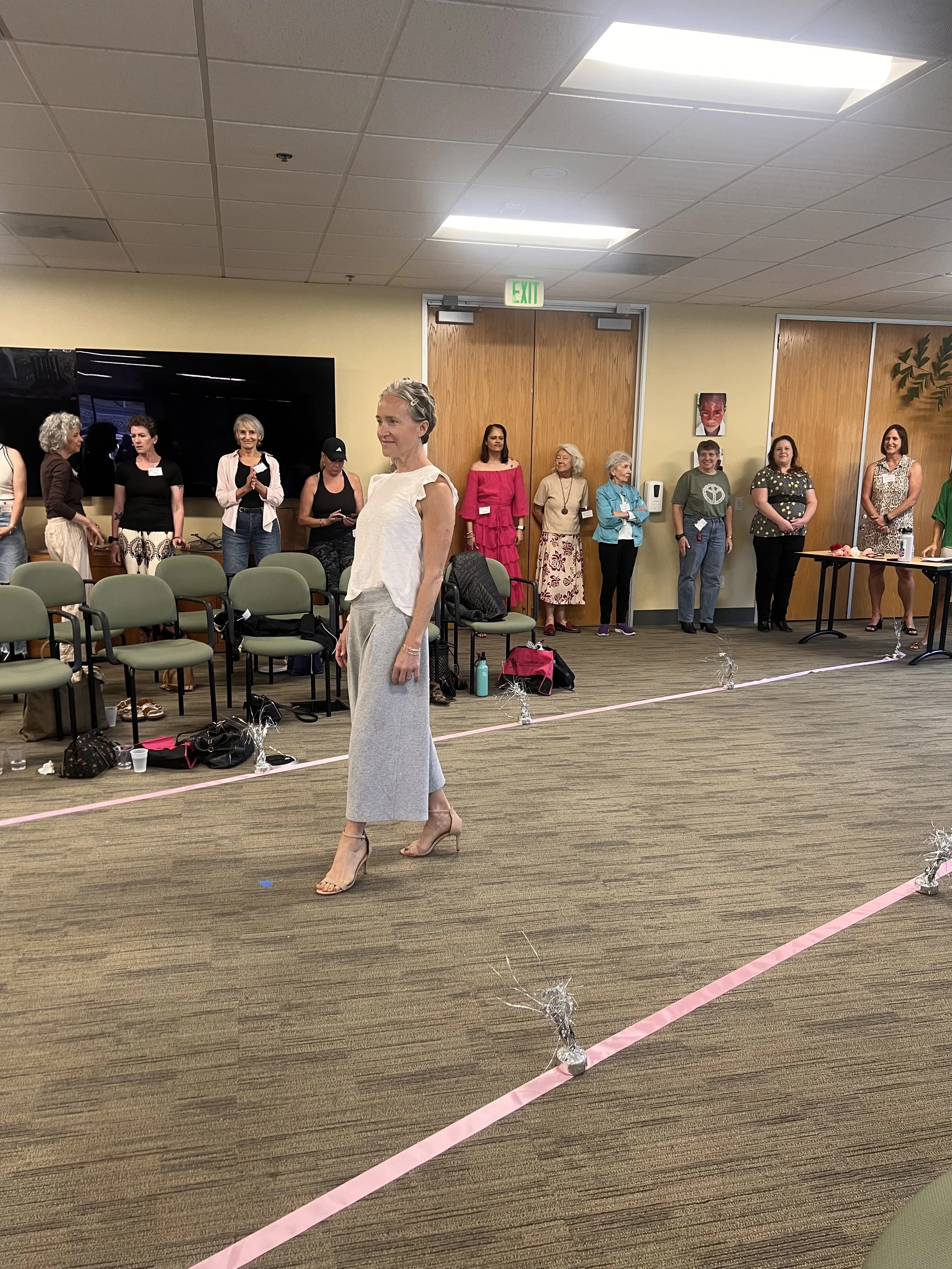
It’s painful, and it’s a drag. I don’t move like the athlete my brain knows I am. I have an amazing trainer and coach who is helping me stay strong like an athlete and keep a good mindset.
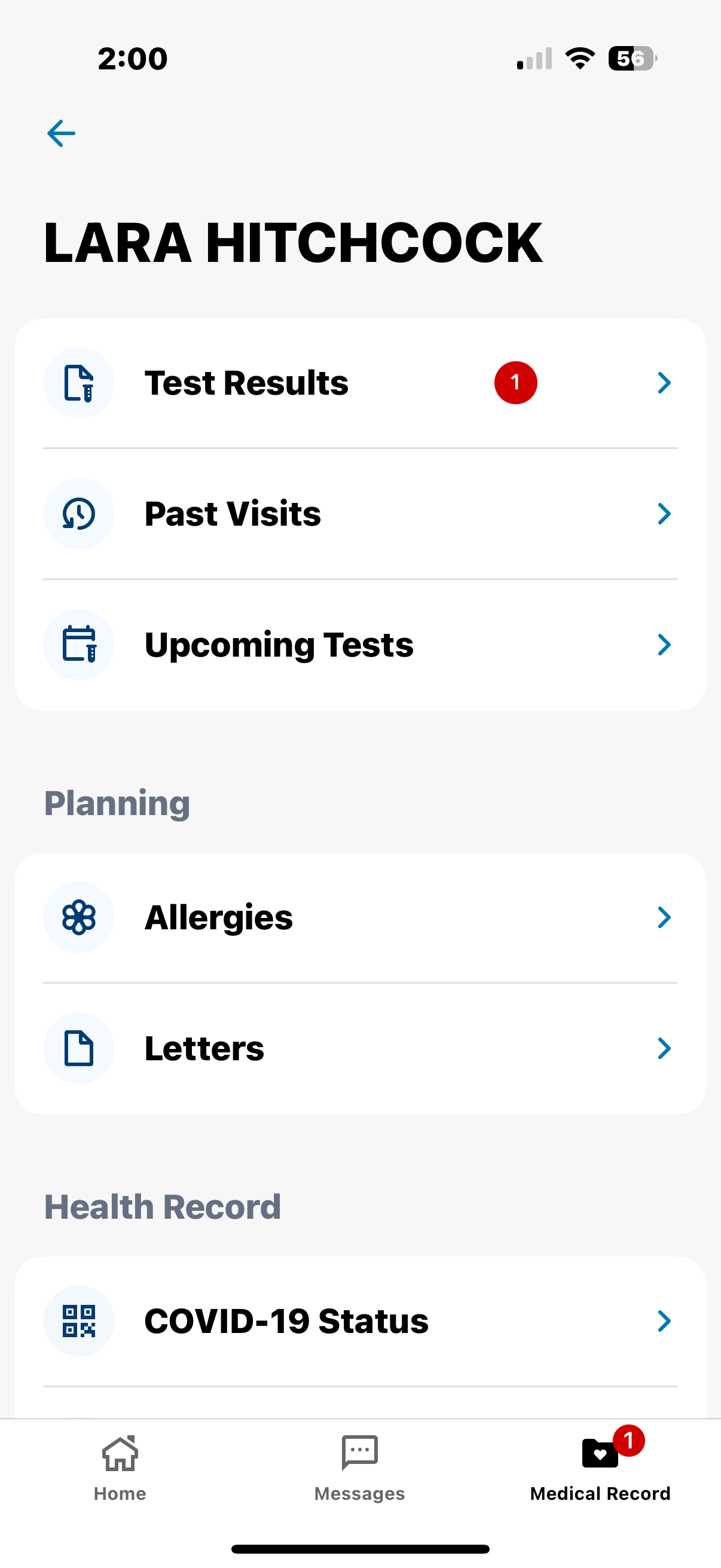
And yet, it feels like the third time in a year that I’ve experienced a sort of identity loss. Chemo was one, Bell’s palsy was another, and now AIs. And the road ahead is long- I’m supposed to be on this treatment for 5,7, or 10 years. It’s only been 7 months.
The other main side effect I experience is hot flushes. I’m using the UK term “flush” v the US term “flash” for two reasons; 1) I love etymology and it appears that flush was first, and 2) it just MAKES MORE SENSE. Theres nothing flashy about sweat.
I have been experiencing 5-10 of these hot flushes every day. Yes, they are super annoying and inconvenient. But I learned pretty quickly to always wear a tank top with sweaters on top, immediately discarding layers whenever I sensed it coming on. I went from being always chilly at work to being the woman in a tank top on the zoom. Classy. But to be honest, I would take 10 hot flushes in a hot second compared to any joint pain.
A few days ago, I noticed that I was getting hot or warm a few times each day, but no flush was happening. So that seems to be a quick response to going off the AI. Nice.
And then there are the side effects one doesn’t necessarily “feel” like osteopenia and worsening lipid panels, again from the lack of estrogen.
But I really am hopeful about this break from the AI and resetting my body before the trying the next one. And I’m hopeful about the future- that during these next few years we find better ways to mitigate the impacts of cancer treatment.
To be clear: I’m so glad to be in remission. AND ALSO I want to feel good in my remission. That’s the whole point, right?!
My early morning walk to shake off the stiffness from Letrozole.